Bone nanocomposites marry strength and compatibility
Artificial bone implants could provide a means of avoiding the pain and limitations of using the patient’s own bone in fracture treatments. Now, researchers in India demonstrate that graphene-oxide nanoflakes can enhance the properties of artificial hydroxyapatite composites to provide supportive scaffolds that encourage bone repair.
“The greatest challenge is to design a biomaterial that should match the properties of native healthy bone,” said Manitha Nair, who produced these latest results alongside colleagues Shantikumar V Nair and Sajini Vadukumpully at the Amrita Institute of Medical Sciences and Research Centre in India. “Properties like biocompatibility, chemical composition, porosity, degradation and mechanical stability are very critical to decide the success of the biomaterial.” Traditionally, bone fractures that fail to heal spontaneously are treated with bone grafts, where the damaged area is replaced with healthy bone harvested from elsewhere in the body. However, this can cause damage to the area where the bone is harvested, as well as significant discomfort to the patient. There are also limits to how much bone material can be obtained this way.
Natural bone is formed from hydroxyapatite – a porous phosphorous and calcium structure – and collagen. However, the expense of obtaining collagen inhibits direct replication of these structures, prompting investigations to determine whether gelatin – a denatured weaker collagen-like material – might be a suitable substitute.
Graphene is renowned for its mechanical strength, among many other material attributes. In their latest work, Nair and her colleagues studied the impact of graphene-oxide nanoflakes in bone scaffolds to assess how they might enhance hydroxyapatite/gelatin nanocomposite bone implants.
Expediting repair
When a fracture mends, stem cells differentiate into osteoblast cells and mend the break. However the stem cells need to migrate from the surrounding area to the damaged site, which can take time, particularly in the elderly who have lower numbers of stem cells.
“It has been suggested that including stem cells into the composite scaffold and implanting them together would alleviate the need to wait for cell migration,” said Nair. However, she goes on to describe the delays accrued with this approach because stem cells need to be isolated from the patient and then multiplied in culture before the implant, all of which can take a few weeks.
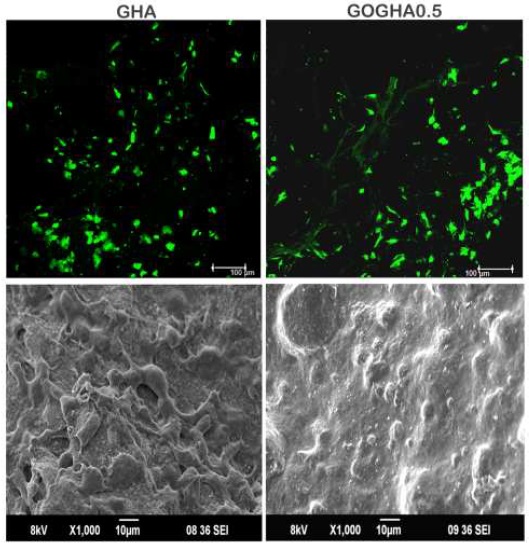
While pristine graphene is prone to agglomerating, graphene oxide has chemical characteristics that can be positively beneficial to cell health while retaining graphene’s mechanical advantages The team cultured mesenchymal cells – which can differentiate into various types of tissue – and monitored the differentiation of these cells into bone.
They found that graphene-oxide nanoflakes greatly expedited the multiplication of stem cells and seemed to encourage differentiation into bone tissue cells. “Usually we need to include supplements,” said Nair. “But even with just the basic culture medium, graphene oxide induces differentiation of stem cells into osteoblasts.”
Next steps
While the team’s preliminary tests have been promising, further work is needed to check the toxicity of graphene-oxide-enhanced hydroxyapatite/gelatin structures. “Graphene-oxide toxicity is a concern because while the constituents of the hydroxyapatite/gelatin scaffold are naturally found in the body, graphene oxide is not and it does not dissolve,” said Nair. “Around 60% of GO was slowly released from the composite scaffold over a period of eight weeks, and that concentration was within the toxicity limit.” She added that bone is more tolerant to graphene oxide than other soft tissue, which is encouraging for the potential adoption of these implants.
Next, Nair and colleagues plan to implant the graphene-oxide-enhanced scaffolds in live animals to test the toxicity, as well as the speed and quality of bone regeneration.
Photo’s captation: Mesenchymal cells derived from human adipose tissue (found in skin fat and bone marrow) on composite scaffolds after 24 h. Upper panel: Confocal micrographs showing the viable cells (green). Lower panel: Scanning electron micrographs showing cell morphology. GHA: gelatin/hydroxyapatite scaffold; GOGHA0.5 gelatin/hydroxyapatite scaffold with 0.5 wt% graphene oxide. Courtesy of Nanotechnology